
Saving lives around the world for more than 50 years
+
employees
%
income from the Czech state budget
+
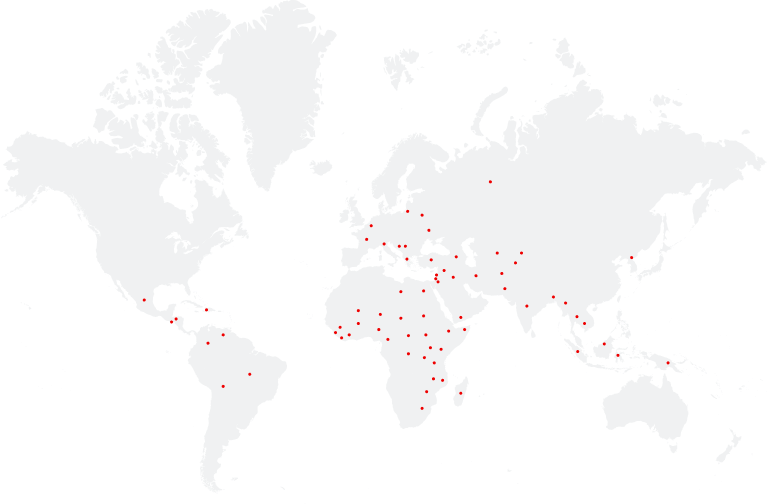
countries around the world
+
projects
mil.
patients admitted annually
Neutrally, independently and impartially.
We are a Nobel Peace Prize-winning medical and humanitarian organisation. We provide assistance to people who are affected by war, natural hazards, epidemics, and exclusion. Neutrally. Independently. Impartially
Save lives with us
Médecins Sans Frontières (MSF) teams treat patients all over the world thanks to more than 7 million donors who contribute every year to our social mission. Become one of them!
Join us on an assignment
If you are a medical or other professional and would like to work with us, register for an information evening. You'll find out everything you need to know about going on an assignment.
Become a donor
Your donations enable us to buy medicines, rebuild hospitals, send doctors where they’re needed, and most importantly, treat patients. Support us with your donation and save lives with us.
Support us in other ways
There are other ways to participate in our work besides direct financial donations, such as providing services or free consultations.
You can also become a volunteer, organise a fundraising event or share our testimonies.
Bearing Witness
Saving lives is our priority. However, we don't want to remain silent about what we see on our missions. That's why we speak out publicly and draw attention to the injustices and crises faced by the people we trea.
"Silence has long been confused with neutrality, and has been presented as a necessary condition for humanitarian action. From its beginning, MSF was created in opposition to this assumption. We are not sure that words can always save lives, but we know that silence can certainly kill."
Dr. James Orbinski, MSF International President, 1999

"Silence has long been confused with neutrality, and has been presented as a necessary condition for humanitarian action. From its beginning, MSF was created in opposition to this assumption. We are not sure that words can always save lives, but we know that silence can certainly kill."
Dr. James Orbinski, MSF International President, 1999



 Donate
Donate



